
Top Foods to Eat—and Avoid—for Migraine Relief
Smart Nutrients and Supplements by Mijung
I. INTRODUCTION: JOURNEY TO FIND FOODS FOR MIGRAINE RELIEF
When Samuel was recovering from his lumbar and cervical surgeries and dealing with chronic pain, his migraines became worse—more frequent, more intense, and harder to manage. Efforts to find foods for migraine relief became our top priority. As someone supporting his recovery at home, I could see how helpless and frustrated he felt when the headaches would suddenly flare up. He had already been through enough. I wanted to help.
So, I turned to food—not just to nourish him, but to reduce the hidden triggers that were making things worse. I started tracking what he ate, what helped, and what seemed to make the migraines more intense. Slowly, I began adjusting his meals based on what I was learning—and it made a noticeable difference. Food is direct intake that can make a direct, responsive result!
In this blog, I’ll walk you through:
The common foods we now avoid that triggered Samuel’s migraines
The foods and drinks that helped calm his headaches
A few gentle product swaps that supported his recovery
These aren’t medical treatments, but they are food-based strategies that worked for us. If you or someone you love deals with migraines, I hope our experience gives you something useful to try and build on.
II. TOP MIGRAINE TRIGGER FOODS TO AVOID
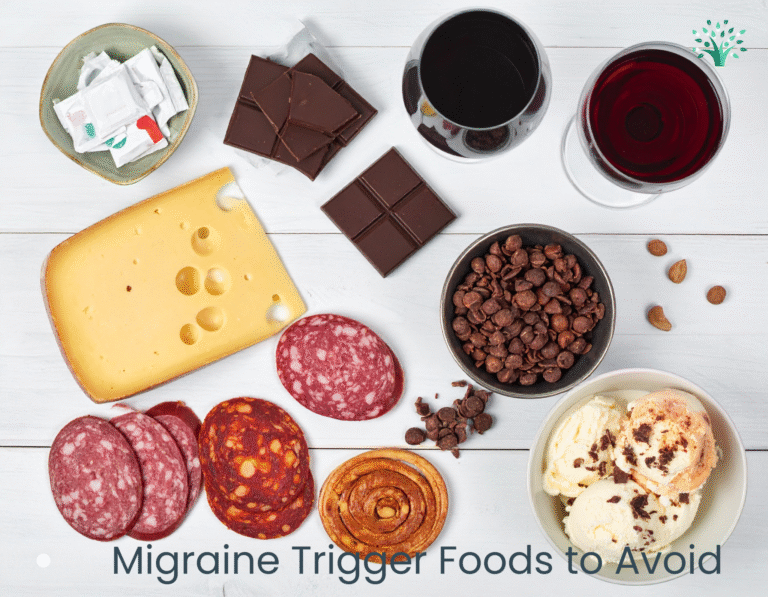
Identifying migraine trigger foods can be incredibly personal—what affects one person may not affect another. However, after carefully logging Samuel’s food intake and symptoms, we noticed clear patterns. These foods consistently led to migraines, especially during stressful periods and pain cycles. (Related post: Pain Management Is Stress Management: My Awakening)
Aged Cheese
Cheddar, gouda, parmesan, and blue cheese contain tyramine, a compound that can influence blood vessel behavior and trigger migraines.Processed Meats
Bacon, sausage, and deli meats are often high in nitrates and nitrites, which can affect blood flow and contribute to vascular migraines.Caffeine
Caffeine withdrawal was one of Samuel’s most consistent migraine triggers. We gradually reduced his intake and made it more consistent.Alcohol (Especially Red Wine)
Red wine contains sulfites and histamines. Even a single glass could lead to a headache, so we eliminated it completely.Chocolate
Though comforting, chocolate contains phenylethylamine, which may cause headaches in some people. We replaced it with magnesium-rich alternatives.MSG (Monosodium Glutamate)
Common in flavored chips, sauces, and restaurant foods, MSG triggered Samuel’s migraines within hours.
Source: Cleveland ClinicArtificial Sweeteners (Aspartame)
Found in diet sodas and sugar-free snacks, aspartame was a consistent trigger. We cut it out entirely.Very Cold Foods or Drinks
Ice cream and freezing drinks—especially on an empty stomach—often caused sudden headache spikes. We now serve food and beverages cool, never icy.
Caregiver Tip:
Keep a food and symptom journal for at least 7 days. Note what was eaten, when, and if any migraine symptoms followed. This simple tracking tool revealed surprising triggers for us—and can do the same for you.
III. TOP FOODS THAT HELP EASE MIGRAINES:
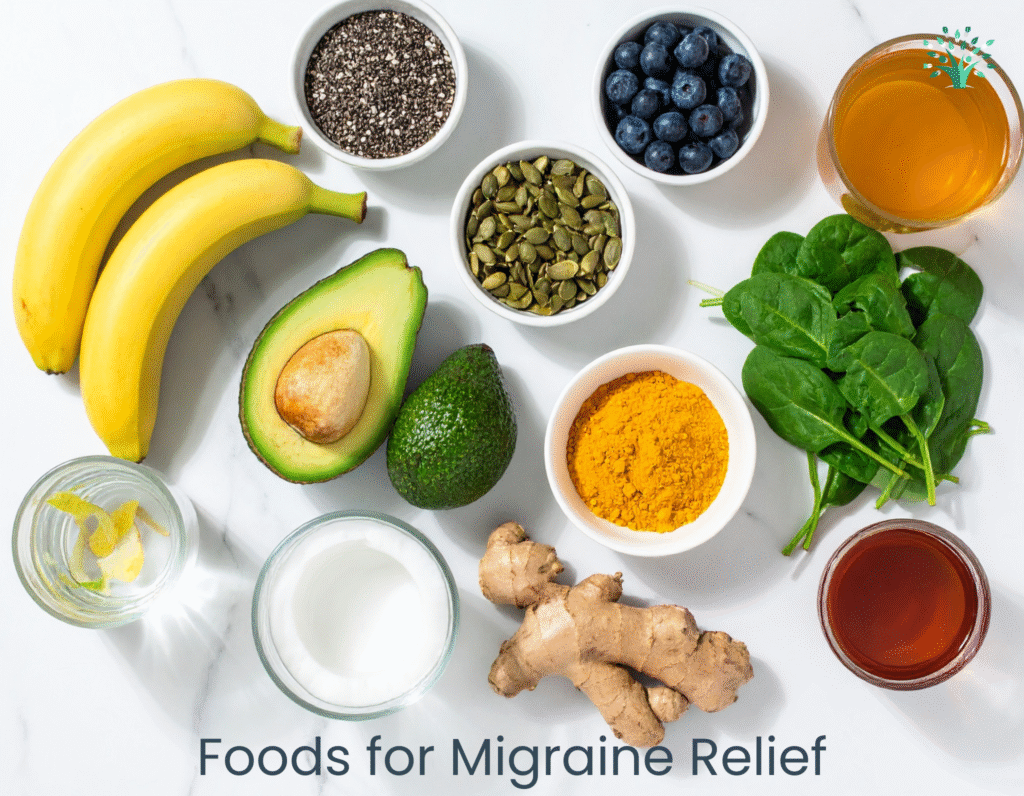
MAGNESIUM-RICH & ANTI INFLAMMATORY FOODS
Once we removed the triggers, I focused on adding foods that would support Sam’s recovery. I looked for magnesium-rich, hydrating, and anti-inflammatory nutrients that could provide relief naturally.
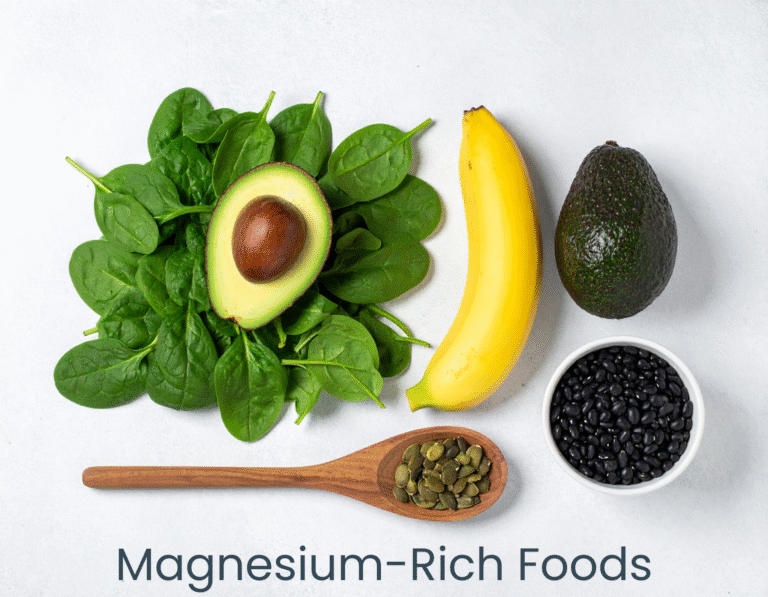
A. Magnesium-Rich Foods
Spinach, avocados, pumpkin seeds, bananas, and black beans became regulars in our weekly meals.
We also added Nature Made Magnesium Glycinate 200 mg—a gentle supplement that supported consistency without upsetting Sam’s stomach.
Source: American Migraine Foundation
B. Anti-Inflammatory Foods
Blueberries, leafy greens, chia seeds, salmon, and turmeric (with black pepper) reduced systemic inflammation and supported his healing beyond migraines.
C. Hydrating Foods & Drinks
Cucumber, watermelon, coconut water, and broth-based soups helped maintain hydration.
Our go-to? Ultima Replenisher Electrolyte Powder – Lemonade. Zero sugar, no dyes, just effective daily hydration support.
D. Natural Soothers: Ginger & Herbal Support
Fresh ginger tea, ginger chews, and soups with ginger all supported Sam during flare-ups.
We still use Traditional Medicinals Organic Ginger Tea. It’s warm, soothing, and helped calm nausea.
Study: Ginger vs. Sumatriptan
Caregiver Tip:
Perfection isn’t required. Just building a few of these foods into your daily routine can noticeably reduce migraine intensity and frequency over time.
IV. WHAT WORKED FOR US – OUR FOOD STRATEGY IN REAL LIFE
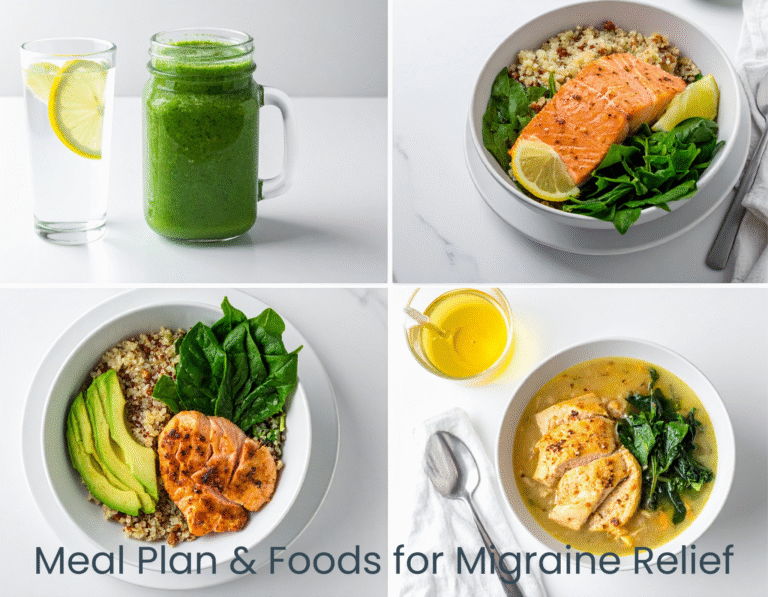
Preview of upcoming blog: One-Day Anti-Migraine Meal Plan (Coming in week of August 4)
Morning Routine:
Warm lemon water
Banana-spinach-chia smoothie with soy milk
Greek yogurt with almonds, walnuts, and blueberries
Bowl of pressure-cooked black beans
Lunch Routine:
Tomato, avocado, broccoli, pan-seared chicken
Ginger tea
Olive oil + lemon dressing salad
Evening Routine:
(Related blog: Energize Your Summer: Korean Ginseng Chicken in the Pressure Cooker)
Ginseng chicken soup
Quinoa, avocado, spinach, and roasted salmon with brown rice
Herbal tea + magnesium glycinate
Light snack to avoid overnight blood sugar dips
Travel/Flare Toolkit:
Ginger chews
Electrolyte packets
Magnesium supplement
Banana
Cooling pack – and for emergencies, the TheraICE Migraine Relief Cap became our go-to for flare-ups. It’s wearable, reusable, and offers instant relief.
V. WHAT’S NEXT IN THIS SERIES

This post is part of our Eat to Ease Migraines blog series:
Coming week of July 21: Can Magnesium Help Migraines? Here’s What to Eat (and What I Use)
Coming week of July 28: Dehydration = Headache: Best Hydration Foods & Drinks for Migraine Relief
Coming week of August 4: One-Day Anti-Migraine Meal Plan: What I Eat to Stay Ahead of Pain
Follow along or bookmark this page. Each entry is grounded in personal experience and backed by nutritional insight.
Affiliate Disclosure:
As an Amazon Associate, we earn from qualifying purchases made through some of the product links in this post. This helps support our blog at no additional cost to you.
vI. FINAL TAKEAWAY - FIND THE RIGHT FOODS FOR MIGRAINE RELIEF

Finding the right foods for migraine relief takes time, tracking, and patience. But when you do find what works, it’s life-changing. The foods Samuel ate—and the ones he avoided—helped reduce the intensity, frequency, and disruption of his migraines more than any single prescription ever did.
Food isn’t a cure, but it’s a powerful tool. If you’re struggling with chronic headaches or migraines, start by tracking your intake, removing triggers, and slowly introducing supportive foods like magnesium-rich vegetables, hydrating fruits, and calming herbal teas. It doesn’t have to be perfect—it just needs to be consistent.
Our journey became our blueprint. I hope it becomes part of yours, too.
— Mijung